News
How will vision loss be treated in the future?
Gene therapy, stem cells, artificial intelligence, the bionic eye – incredible advances in research and technology are opening up new frontiers for eye health.
It’s a brave new world of scientific discovery and futuristic technology. With each step forward, eye researchers are unlocking exciting possibilities for earlier detection of eye disease, better treatments and potentially even restoring sight.
At the Centre for Eye Research Australia’s Looking to the Future Community Forum, held in October 2019, a selection of CERA’s leading experts discussed the current eye research landscape and what the future holds.
Over two panels – ‘Gene therapy demystified’ and ‘Everything you need to know about artificial intelligence and new technology’ – they explored everything from the bionic eye, to corneal cells grown from skin, to computer programs that can detect eye disease with better-than-human accuracy.
Here is a snapshot of some of the key ideas discussed, and the areas of research shaping the future of eye health.

“With the right support, I believe we will be able to make an impact on previously untreatable diseases,” says Professor Keith Martin.
Gene therapy
Our genes determine how our body works, and when a tiny building block is missing or isn’t quite right, it can cause significant problems.
There are over 300 different genes that are known to cause inherited retinal diseases (IRDs) – genetic eye conditions that can lead to vision loss and blindness.
Unfortunately, not much can be done to reverse or slow the progression of these conditions. But gene therapy is opening up a potential pathway to treatment.
“One of the things we’re trying to do at CERA is establish a Melbourne Centre for Ocular Gene and Cell Therapy,” said Professor Keith Martin, CERA Managing Director.
“It’s a really exciting time with new technologies developing. With the right support, I believe we will be able to make an impact on diseases that have previously been considered untreatable.”
In its simplest form, gene therapy for eye disease works by identifying a defective gene which causes vision loss, producing a correct copy in the lab and reintroducing it to the eye using a specially-engineered virus.
“The virus is a bit like an envelope that we put a message inside,” Professor Martin explained. “The virus sticks onto the cell, and the cell reads the instructions for the little building block it’s missing.”
The world’s first ocular gene therapy, for a rare inherited retinal disease, has been approved for clinical use in the US and Europe. It’s anticipated that many more gene therapies will become available in the next few years.
“With the right support, I believe we will be able to make an impact on diseases that have previously been considered untreatable.”
So what possibilities does this offer to someone living with an inherited retinal disease?
Dr Tom Edwards, CERA’s Principal Investigator in Retinal Gene Therapy Research, said it’s important to understand that these therapies need to be developed specifically to the gene that’s causing the problem.
“The first step is to try to identify the gene that’s causing the condition, which we can generally do in 70-80% of cases,” he said. “Once you know the gene, you can then look online to determine if there are any groups working on gene therapies for that particular gene.
“You can also get in touch with CERA so we know about your condition, so that if a potential treatment becomes available, you’re ready to get involved.”
Genetic counselling can help you navigate these practical and often emotional issues, added Lisa Kearns, CERA orthoptist and associate genetic counsellor.
“Often when someone is diagnosed with an inherited retinal disease, there are a lot of emotions,” she said. “They’re shocked and overwhelmed, and they have a lot of questions. It’s very important to have genetic counselling to talk about these issues.”
“We can refer patients and families to support groups and agencies so that they can make the most of their vision with aids and technology. We can help make sure the appropriate paperwork is completed – for example, if they meet the criteria for legal blindness.
“And we can discuss what research opportunities might be available to you – if there is a clinical trial or a research study that might be suitable for you.”
In Victoria, families with inherited eye diseases can be referred to the Ocular Genetic Clinic (OGC) within the Royal Victorian Eye and Ear Hospital (RVEEH). This clinic is a partnership between the RVEEH and Royal Melbourne Hospital (RMH) genetics service.
Beyond inherited retinal diseases, there is also potential for gene therapy to be used to treat more common eye diseases like glaucoma. This is a particular area of interest for Professor Martin, one of the world’s leading glaucoma specialists.
“However, using gene therapy for glaucoma is much trickier,” he said. “There are many different types of glaucoma, and most of them don’t just involve one gene.
“So rather than putting in a missing gene, we’re investigating gene therapies to boost up the protective pathways within the cells of the eye, to make them stronger and more resistant to damage.”
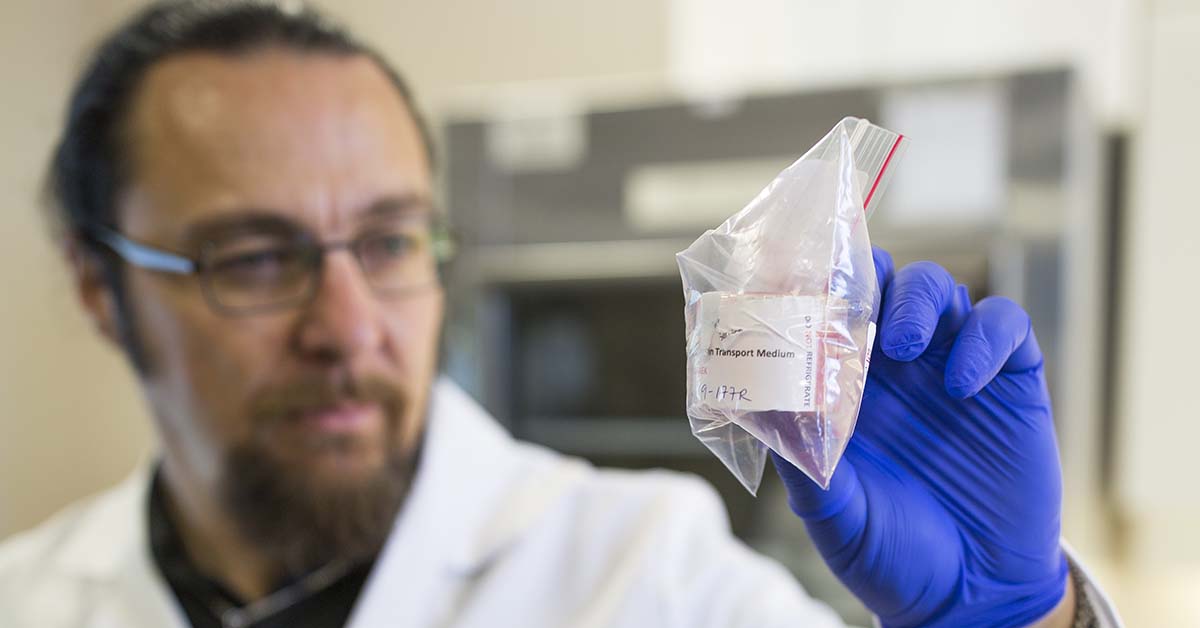
CERA researchers are developing stem cell technologies that can replace the inner cells of the cornea.
Stem cell technology
Stem cell technology is developing rapidly, and research into the eye is leading the way. At CERA, researchers are developing stem cell technologies that can replace the inner cells of the cornea, the clear window at the front of the eye.
This layer of cells keeps the cornea clear, but in conditions such as Fuchs’ dystrophy the cells degenerate, impacting vision. Currently, this can be treated with a corneal transplant, which relies on corneas being donated by people after their death.
“With stem cell technology, we can now grow those cells and attach them to an artificial membrane,” Professor Martin said. “The advantage of this technology is that we can produce enough cells from one donor to potentially treat a large number of people.”
Similarly, there is a lot of research investigating treatments for macular degeneration, using stem cells derived either from donors or, more recently, from skin cells from the patients themselves.
“Believe it or not, you can turn cells from your skin into pretty much any cell in the body, using technology that was developed a few years ago,” Professor Martin said.
“Stem cell technology allows us to turn mature cells back into stem cells, their more primitive state. From there, they can be developed into any of the different specialised cells in the body, depending on what instructions you give them.”

“We’ve been working on a device that we place within the eye, for patients with retinitis pigmentosa,” says Associate Professor Penny Allen.
The bionic eye
Restoring lost vision completely may never be possible. But remarkable advances in the development of a bionic eye bring new hope that blind patients could one day regain some functional sight.
At CERA, a new bionic eye prototype has given four blind patients a ‘sense of vision’ – the ability to detect edges, shapes and movement to aid them in navigating the everyday world.
“A bionic eye is a device that can use electrical or light energy to stimulate visual impulses in patents who are otherwise severely visually impaired,” said Associate Professor Penny Allen, leader of the Bionic Eye Project at CERA.
“We’ve been working on a device that we place within the eye, for patients with retinitis pigmentosa, which is an umbrella term for many inherited retinal diseases. We are currently on our second trial, with four patients.”
Each of these patients has been unable to navigate independently for at least 15 years. The device gives them flashes of light that they are learning to interpret, helping them to identify objects.
“It takes persistence. All of our patients work really hard and we’re really pleased that they’re getting results that they feel are helpful,” Associate Professor Allen said.
“The plan for this second trial is to try to determine whether the device becomes more useful to the patients if they use it more frequently, for example at home and in situations outside the lab.”

“Artificial intelligence is an umbrella term for computer programs that simulate aspects of human intelligence,” says Associate Professor Peter van Wijngaarden.
Artificial intelligence
It might conjure images of science fiction, but artificial intelligence has very real applications in medicine.
“Essentially, artificial intelligence is an umbrella term for computer programs that simulate aspects of human intelligence,” said Associate Professor Peter van Wijngaarden, CERA Deputy Director.
“In the last two decades, artificial intelligence has related to what we call machine learning – where a computer system is trained to learn some functions on its own.
“And in the last decade, a new form has emerged called deep learning, which is modelled on the way memory and learning work in the brain.”
One example in eye health is using deep learning algorithms to analyse images of the back of the eye, looking for signs of disease.
“In early 2015, we started developing a deep learning algorithm that can detect changes in the retina, the back of the eye, due to diabetic retinopathy, glaucoma, macular degeneration and cataract,” explained Dr Jane Scheetz, CERA research fellow.
“Through our trials it’s been found to be highly accurate, greater than 95%. Our next move was to test it in real-world settings – in GP and endocrinology clinics and Indigenous health settings.”
The idea is that rather than needing an ophthalmologist or optometrist to perform an eye health screening, a nurse or Indigenous health worker could use this technology to take a quick image of the eye, and easily identify if a patient needs to be referred to a specialist.
In remote and rural communities, where eye health care can be difficult to access, this could make a profound difference.
“We know that Indigenous Australians are far less likely to have their eyes tested, and they are also almost twice as likely to develop diabetic retinopathy,” Dr Scheetz said.
“This is the big impact I feel artificial intelligence can have – for those people who don’t have access to eye health care.”
