Research
Innovation times four
Four inventive new ideas to transform eye care have received a kick-start from the CERA Innovation Fund.
In 2022, Associate Professor Elaine Chong, Dr Sandy Hung, Associate Professor Guei-Sheung (Rick) Liu and Dr Jennifer Fan Gaskin received funding for research projects that are taking a new approach to tackling eye disease.
From developing eye drops to replace eye injections to a virtual eye model to educate patients about eye disease – each project is taking a novel approach to addressing long-standing challenges.
CERA Business Development Manager, Dr Shereen Tan, says the Innovation Fund aims to support research at critical stages, giving scientists support to gather the data or evidence they need to be competitive in government schemes or attract industry investment for their research.
“The Innovation Fund supports researchers who want to take their ideas from the lab to the clinic to improve patient care – with extra funding for patent applications, pre-seed funding for start-ups and other early operating costs for companies incubated at CERA,” says Dr Tan.
The Innovation Fund was established in 2017 from the generous philanthropic support of the estate of the late Ruth Chitty.
The fund was bolstered in 2021 when CERA added proceeds from the sale of its first spin-out company, Oculo, to create a dedicated, sustainable pool of funding to support innovative vision research into the future.
Easing the eye injection burden
To alleviate the burden of frequent eye injections, CERA’s Head of Genetic Engineering, Associate Professor Guei-Sheung (Rick) Liu, is investigating the development of a new gene therapy that could be delivered as a long-lasting injection, or via an eye drop.
“People with age-related macular degeneration (AMD) or diabetic retinopathy have abnormal blood vessels growing in their retina, the light-sensitive layer of nerve tissue at the back of the eye,” explains Associate Professor Liu.
“These new blood vessels are not very strong and can leak – causing damage to the retina that will eventually lead to vision loss.
“But the regular injections required to stop this abnormal growth are invasive and expensive to both patients and the healthcare system.”
Associate Professor Liu’s research involves changing a protein involved in blood vessel formation.
Driving more genetic passengers
Gene therapies are offering new hope for people living with inherited retinal disease.
In clinical trials, the most common way to deliver retinal gene therapies is using a virus known as AAV.
The AAV vector is a safe virus which enables the correct gene copies to be introduced into cells.
However, Dr Sandy Hung, Research Fellow in Clinical Genetics, explains that up to two thirds of the genes associated with IRDs are too large to fit into one AAV vector.
“Trying to get larger genes into the retina with an AAV vector is like trying to get a group of people to a destination in a taxi when you need a bus,” she says.
Dr Hung aims to develop delivery systems large enough to carry bigger genes that can effectively target retinal cells. Initially the research will target the light-sensing photoreceptors.
“This will help us develop more treatments for IRDs,” she says.
One Right Eye
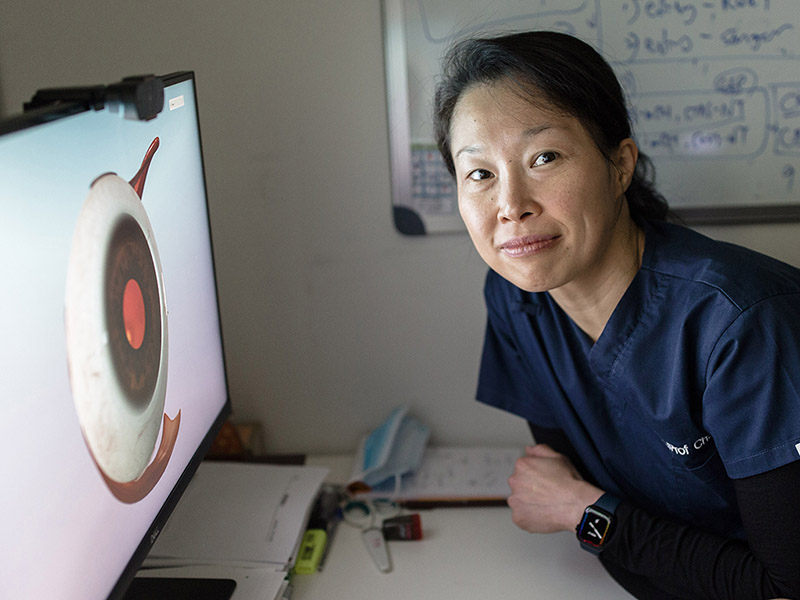
Anatomical eye models can help clinicians describe eye conditions to patients, but they are expensive, fragile and often unavailable in many hospitals and clinics.
This is a scenario Associate Professor Elaine Chong, Senior Research Fellow in Corneal Research, is all too familiar with.
“When explaining a condition like cataract or glaucoma to patients, you’re often trying to provide them with a conceptual understanding of something that is difficult to explain with words alone,” she says.
This often results in confusion for the patient and frustration for the clinician.
To provide patients with a better understanding, Associate Professor Chong and co-founder Dr Joos Meyer, an ophthalmology trainee, developed a virtual 3D eye model.
An initial grant from Telematics Trust led to Associate Professor Chong and Dr Meyer working with a team of designers and artists to develop One Right Eye, modelled on a human right eye.
The software allows clinicians to visually demonstrate the potential damage caused by cataracts, diabetic retinopathy, glaucoma and AMD.

Stopping scarring
The use of anti-VEGF injections have revolutionised how wet AMD is treated.
However, many who receive these regular injections continue to lose their vision, with one contributing factor being scarring in the retina.
“Scarring is a source of disease for almost every part of the eye,” says Dr Jennifer Fan Gaskin, Principal Investigator, Ocular Fibrosis.
“We want to try and go straight to the source to stop it.”
Working alongside Associate Professor Liu and Professor Robyn Guymer AM, Dr Fan Gaskin is conducting research to develop a gene therapy to this end.
She is aiming to disrupt the process that causes scarring to prevent the buildup of tissue that threatens sight.
“This process would require only a one-time injection, while providing a long-term effect,” says Dr Fan Gaskin.
This story was originally published in See the future: Annual Review 2022.
